Front Page
After 20 Years of Kneecap Dislocations, Back to Sports, Pain Free
Drs. Marci Goolsby and Beth Shubin Stein Named New Co-Directors of the HSS Women’s Sports Medicine Center
Patella dislocations- what we know and what we don’t
Having a patella dislocation can be a very scary and stressful injury for patients. While any injury can be difficult to deal with, in my experience patella dislocations in particular can be anxiety producing for patients because there is the fear of the unknown – the fear that their patella will dislocate again or the fear that it will happen to their other knee, and how this will affect their ability to continue playing sports or go to school or work. It also conjures up thoughts of needing surgery. The injury can happen from a contact injury, such as colliding with another player during a soccer game, or from a sudden twist or turn. The injury happens very quickly and in some instances the individual may fall to the floor and they may be unable to walk. Their knee may get very big and swollen, and they may end up in the emergency room in order to get their patella relocated. Then they are typically sent home with a brace and instructed to see an orthopedist who specializes in patella injuries like myself. This may be the individual’s first time having such an injury or they may have had recurrent episodes of the patella “shifting” but not dislocating in the past, or this may be the tenth time their patella has dislocated. Regardless of the circumstances, this injury can take a psychological toll on patients and understandably so.

I have dedicated my career to understanding the complexities and intricacies of the patella and there is still a lot we have to learn. I have authored books and done extensive research on the subject of patella instability and pain and have helped develop systematic approaches to the surgical management of these injuries including medial patellofemoral ligament reconstruction (MPFL). I have performed countless surgeries to correct these injuries and have had excellent results and success. Despite all my efforts there is still a lot we don’t know when it comes to selecting the right patients for surgery. For example, a 16-year-old competitive soccer player who comes into my office with her parents after her first patella dislocation during a soccer game. They are devastated by her injury and they may want to have the surgery done as soon as possible to maximize recovery time so as not to miss the following season. The anxiety and tensions are obviously very high, and we have an extensive conversation about patella instability including why the injury likely happened, what the risks are that this will happen again and what I feel is the best approach to managing her injury. Then comes the most difficult part of the conversation, which is that we know that MPFL reconstruction is a safe and effective procedure but what we don’t know for certain yet is whether or not a first-time dislocator should have surgery. The standard of care currently is that non-surgical treatment is the best option for first-time dislocations unless there are other related injuries such as a displaced piece of cartilage in the knee. Explaining to a 16-year-old competitive soccer player and her family that she has a high risk of another dislocation but that she should be treated without surgery is a very difficult conversation to have. This is why I have dedicated years to my current research studies to be able to make a more informed decision with my patients. I am leading a study that aims to answer whether a young first-time dislocator should be treated with surgery called PAPI (Pediatric and Adolescent Patellar Instability). This is a multi-center study in which patients who are selected randomly to either be treated with surgery or without surgery after their first patellar dislocation. Another study that I am leading called JUPITER is a large multi-center patient registry on patellar instability and is the first of its kind in the US. We currently have 28 orthopedic surgeons at 13 centers across the country contributing to JUPITER, and to date have enrolled over 1,200 patients with patellar instability. In the not too distant future, the hope is that the results of these studies will give us a clearer picture of how we should be managing first-time dislocators and patella instability in general, and will allow me to be able to have a more informed conversation with my patients and their families and help to alleviate some of their anxiety and concerns.

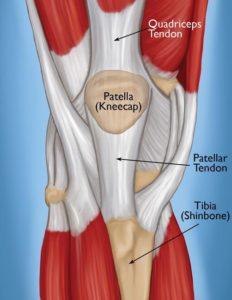
Spotlight Patella: Interesting facts about this simple yet complex structure in our knee.
Did you know ostriches are born with four kneecaps (patella)? The evolutionary reason for this is still not fully understood but theories include that it allows this heavy fast bird to straighten its knee faster thereby helping it to run faster. I have dedicated so much of my career to issues of the human patella. Many issues can arise from this small but fascinating bone. See below to learn some fun facts about this simple yet complex structure in our knees.
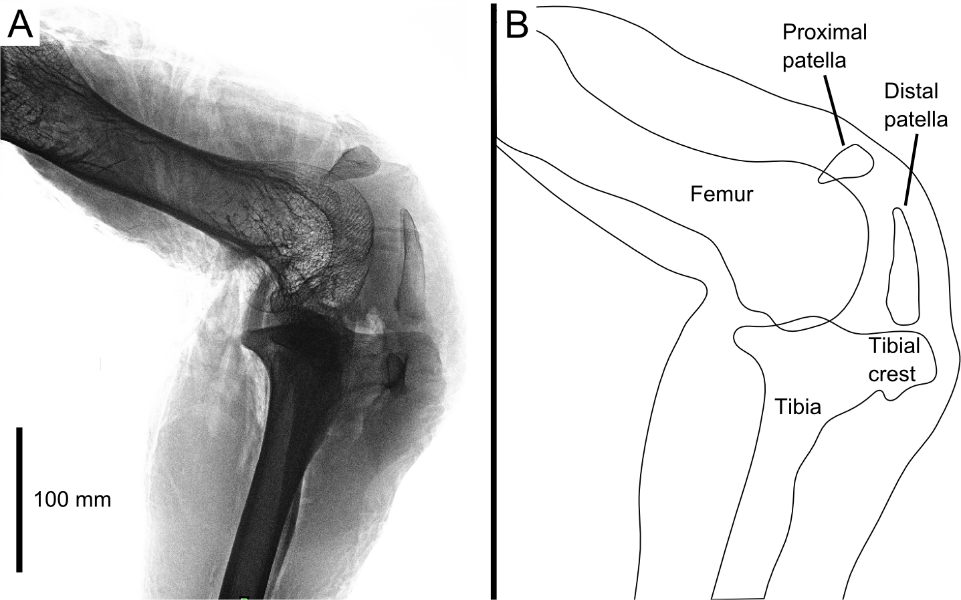
- The patella is a roughly triangular shaped bone called a sesamoid bone from the Latin sesamun “sesame seed”. It is the largest of this type of bone in our body as compared to the tiny sesamoid bones in say our foot.
- Babies are born with a patella made of cartilage instead of bone partly due to its flexibility for the birthing process
- The patella slowly turns from cartilage to bone between the ages of 2-6 years old
- Some people’s patella bone never fuses and so they may have two separate bones know as a bipartite patella. Rare genetic disorders cause some people to not develop a patella bone.
- “The knee bone is connected to the thigh bone” – this is sort of true as the quadriceps tendon in your thigh attaches to the upper part of your patella and patella tendon below your patella attaches to your shin bone.
- The patella sees an average of 2.5-3.5 times your body weight with stairs and up to 7-8 times your body weight with deep squat.
- The patella is vital to protect the inner structures of your knee acting as a shield. The patella increases the leverage of the knee extensor (straightening) muscles, so they don’t need as much force to straighten the knee.
- For such a small bone it is prone to injury including fractures, dislocations, patellofemoral syndrome and arthritis. Some people even have the patella removed due to severe injury or arthritis.
These are just some of the interesting facts about the patella and demonstrate how intricate and fascinating a structure it is in our bodies. Given that injuries to this bone and surrounding tendons, ligaments and joints are so common, it is important to properly manage these injuries to prevent damage to the surrounding structures as they are all interconnected. If you are experiencing issues of the patella or patellofemoral joint please visit the patellofemoral disorder section of my website to learn more.
By Dr. Beth Shubin Stein

I am double jointed. Does this mean I have more joints that other people?
The term double-jointed is a misnomer. The name implies that a person has twice the number of joints as normal and thus their joints allow for greater movement outside of the normal range of motion for that joint. What this term actually refers to is that a person has greater mobility or flexibility of their actual joint and can move their joint beyond its normal end range without experiencing pain and discomfort. Hypermobile joints tend to be inherited. It occurs in about 10-25% of the general population.
Most people don’t experience any symptoms and don’t need any intervention, but a small percentage of patients will have hypermobility syndrome where their unstable joints can lead to other conditions. Some may experience frequent sprains or tendinitis of their joints and activity modification and physical therapy may be recommended to strengthen and stabilize their joints. In some rare cases, these joint issues may be related to a more serious underlying medical condition. In my practice, I often see patients who experience subluxations or dislocations especially of their knee cap (patella) or their shoulder joint due to hypermobility. A subluxation is when the bones of a joint partially move out of place and then relocate back in on their own (known as a partial dislocation) versus an actual dislocation where the bones move completely out of the joint and stay out until relocated. These injuries may occur from direct trauma to the joint like during sports or from a fall.
I routinely see another subset of patients in my practice who have abnormal joint anatomy where the ends of their bones in their joint are abnormally shaped. These patients can not only have laxity in their joints but also have anatomy that predisposes them to injury. These patients can experience a subluxation or dislocation event even without trauma such as from a sudden twist or movement of their joint. These patients require a thorough evaluation to determine what the best treatment is for them. It can range from pain medication and physical therapy to surgeries to stabilize the joint and prevent re-injury. Having hypermobile joints is not a problem for most people, but if pain and frequent injuries occur it is important to see an orthopedist who regularly deals with these issues.
My teammate had an ACL repair, why is a different ACL surgery being recommended for me?
Over the years in my practice, this has become a familiar question—many patients come to my clinic wondering about their options for anterior cruciate ligament (ACL) surgery. These patients range from someone who tripped and fell to recreational athletes who sustained an ACL tear skiing, to the amateur/professional athletes who sustained an ACL tear competing in high-level, pivot-heavy sports. My first response to my patients is that there is no one-size-fits-all approach to ACL surgery. I begin by explaining the difference between an ACL repair (where the ligament is sewn back to its origin) versus an ACL reconstruction (where a new ligament is constructed for them). We discuss that every case is unique and that there a multiple factors that go into determining the right type of surgical or non-surgical solution for their ACL injury, including:
- Location and type of tear:
Most ACL tears occur in the middle or mid-substance of the ACL, and can be partial, meaning part of the ligament is torn, or complete, where the ligaments is torn in half. Less frequently we see an avulsion type ACL injury, where the ACL “peels off” from its attachment to the bone. These injuries are all ACL tears, but the treatments are not all the same.
- Chronicity of the tear:
We want to know if this is a recent ACL injury, or if the ACL injury occurred months to years ago, as this affects healing patterns.
- Age & activity level:
The age, activity level, and future expectations of the patient are each critical factors in determining the right approach to ACL surgery. Is the patient low demand, meaning they want to get back to bike riding or yoga or are they high demand college athlete competing in cutting and pivoting sports.
- Surgical history:
I am looking to determine what prior knee surgery the patient has had on the injured knee, as well as the other knee and joints.
- Imaging results:
These results help us see if there is a fracture or break in the bone where the ACL attaches, a tear in the meniscus (shock absorber), damage to the cartilage (smooth glossy coating over the bones) and damage to other ligaments. These factors also affect the type of treatment that may be needed. - Physical exam results
This includes an evaluation in the office where we assess areas of pain and other stabilizing ligaments in your knee to see how stable your knee is. We also examine the anatomy of your knee to ensure proper alignment and mobility of your hips, knees and ankle joints.
These are just some of the factors that go into making the appropriate treatment choice to heal your ACL injury. While your friend, colleague or teammate may have had a different approach and experience with their ACL injury treatment, it doesn’t mean yours will be the same. Having a detailed discussion with your doctor about your options and coming up with a plan that works best for you is ultimately the most important factor.